Disease Information
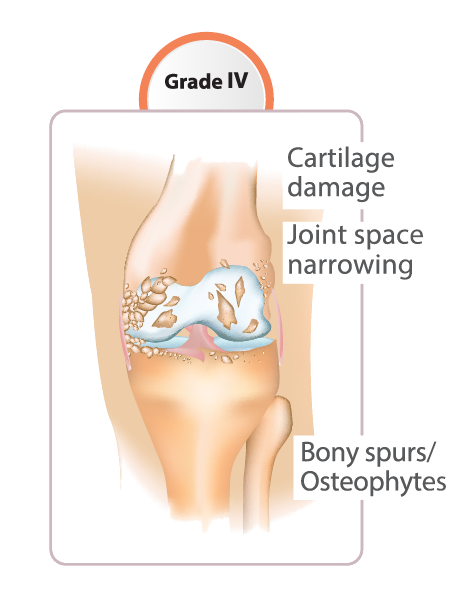
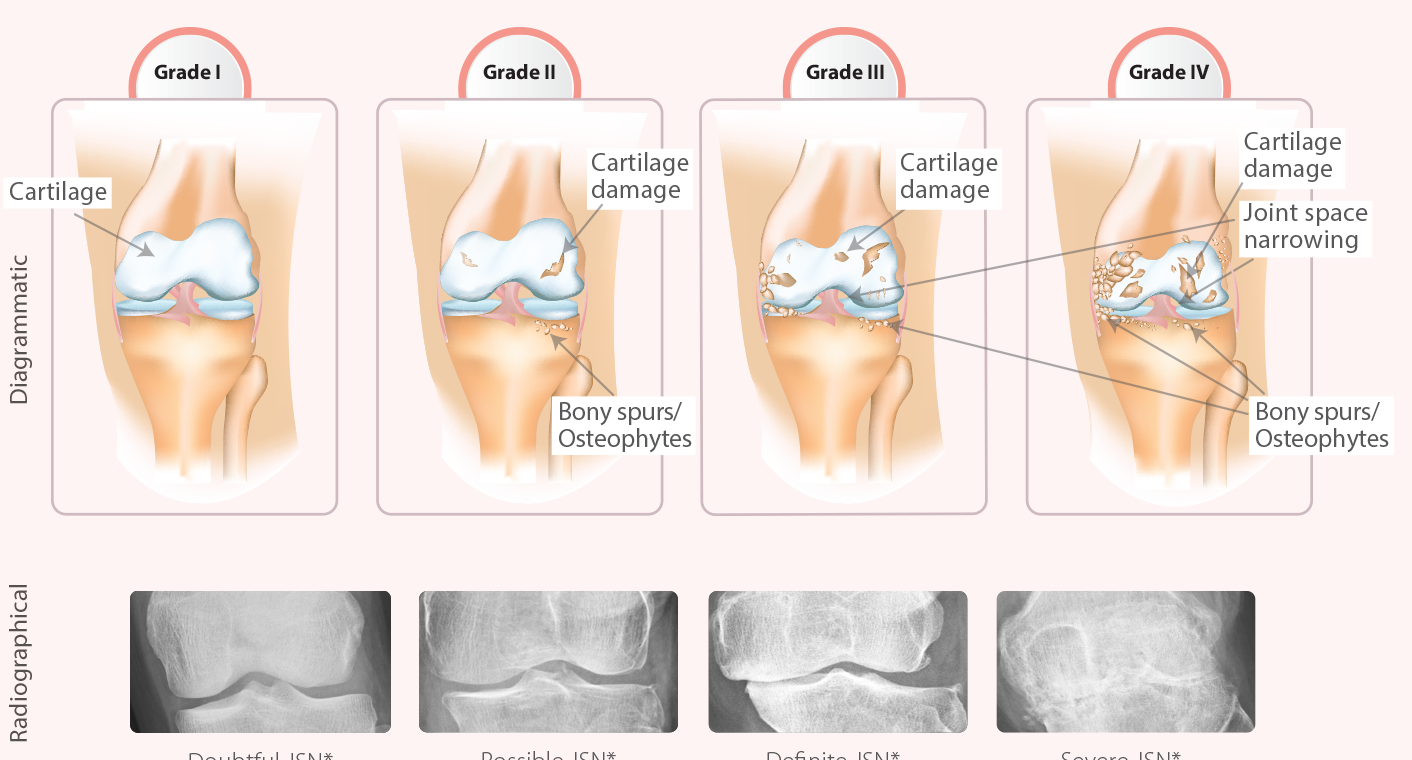
1. A chronic, progressive musculoskeletal disorder characterized by gradual loss of cartilage in joints, which results in bones rubbing together and creating stiffness, pain and impaired movement
2. Worldwide, some degree of knee OA is likely in 10-15% of people >60 years of age
3. Radiological evidence of knee OA observed in ~70% of woman > 65 years of age
4. As per the National Health Portal of India report,22-39% of Indians are affected by knee OA
5. Knee OA, the commonest type of arthritis, typically caused due to wear and tear and progressive loss of the articular cartilage